Could anti-obesity meds help troops’ weight issues?

As his years in the military progressed, Shaun Gamble began finding it harder and harder to keep his weight in check.
Gamble, 46, characterized the last few years of his nearly 25-year career as a struggle to stay in fighting shape.
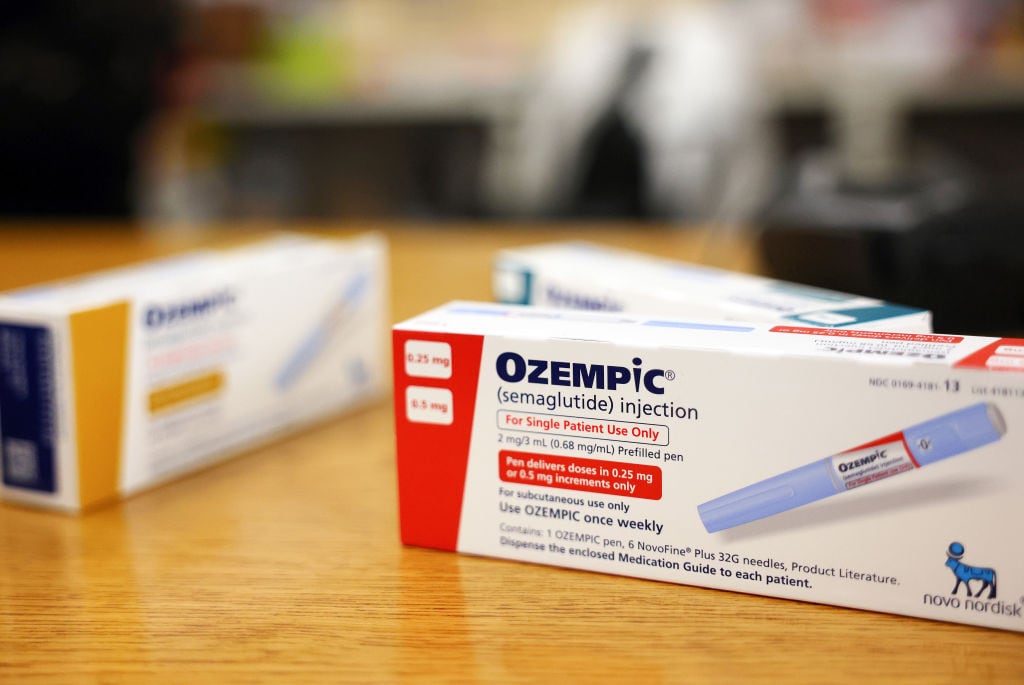
That changed in April 2023, when a civilian doctor prescribed him Ozempic. He soon shed 44 pounds, he told Military Times, getting down to about 200.
Gamble was medically separated from the Kentucky Army National Guard, retiring as a master sergeant earlier this year. He alleges his discharge was in part due to taking a personal route toward acquiring and using Ozempic, instead of going through military-approved channels to get the prescription.
But despite how his career concluded, Gamble is clear about one thing: Ozempic, a weight-loss drug now sweeping the nation, helped get him into shape.
“As soon as I started taking the Ozempic, it just kind of toned me up pretty quick,” he said.
Gamble’s struggles with weight are not unique.
The U.S. military needs its troops in fighting shape to carry out the mission, but like many other Americans, service members have become heavier in recent years.
More than two-thirds of active duty troops are now considered overweight or obese, Military Times previously reported, citing a study by the American Security Project, a nonpartisan research organization.
RELATED
Anti-obesity drugs like Ozempic can offer troops fast weight loss, and their use has grown across the ranks in recent years, even as some researchers argue that the military brass is not using them as much as they could.
At the same time, while usage has increased, the military is in short supply of policies that determine when such drugs should be prescribed.
Some researchers argue that the military health care system should be taking advantage of drugs like Ozempic to improve service member health, refine military readiness and reduce fiscal costs associated with being overweight or obese.
Military officials have publicly expressed concern about how an overweight force endangers the mission. Active-duty service members struggling with obesity are 33% to 47% more likely to suffer musculoskeletal problems, contributing to injuries, impaired readiness and possible medical separation, according to a Defense Health Agency-funded study published in August.
But problematic health trends also pose financial burdens shouldered by the Defense Department.
Service member obesity costs the Pentagon more than $1.35 billion annually, with direct care costs in 2023 accounting for $1.25 billion and productivity losses — due to hospital stays — costing an additional $99 million, according to a separate report by the American Security Project.
Promises and perils
Drugs like Ozempic work in part by regulating one’s appetite. And while makers of the drugs have warned about side effects, which occur with other medications as well, experts note that long-term impacts still need to be explored.
Many of the drugs have long been used to treat diabetes, but their use as weight-loss wonder medications — lifetime use is required to maintain a lower weight — is relatively unchartered territory.
Ozempic isn’t approved by the U.S. Food and Drug Administration for weight loss, but is sometimes prescribed off-label to help people lose weight. Wegovy, Saxenda and Zepbound are among FDA-approved options for weight loss.
Some studies warn of pitfalls that can occur when trying to transition away from using the expensive medications, including the regaining of weight, NPR reported. And as their popularity has grown, some Americans remain dubious.
A Pew Research Center survey conducted in February examined American attitudes toward weight-loss drugs and found that, while more than half of those familiar with the medications consider them a valuable weight loss option, 19% believe they are not, while 28% are unsure.

The military’s Tricare health program began approving coverage of FDA-approved weight-loss medications in May 2018. And while associated prescriptions in the ranks have dramatically increased since, they are still being used by a small percentage of the force.
The prevalence of weight-loss prescriptions in the active component increased from 1.2 per 100,000 service members in the first quarter of 2018 to 104.4 in the second quarter of 2023, a recent study by Medical Surveillance Monthly Report noted. That dramatic surge involved prescriptions increasing from seven to 816 during the study period.
Less than 1% of active duty personnel currently use anti-obesity medications, according to the Defense Health Agency-funded report.
But that report’s authors contend that at least 22% of the active duty population would qualify for the medications because they meet body-mass index criteria for obesity. In fact, the prevalence of those considered overweight and obese within the Military Health System is 41.6% and 30.5%, respectively, the study notes.
Researchers and analysts outside the military argue that a pervasive weight bias in the military, along with a confusing and administratively burdensome system of authorization, play into a lack of wider adoption of the drugs.
They also point to a lack of obesity training and education for providers and a limited nationwide supply as factors.
Such issues have been top of mind for some military leaders of late.
Marine Sgt. Maj. Troy Black, senior enlisted advisor to the chairman of the Joint Chiefs of Staff, said during a podcast interview this summer that removing fast-food restaurants from military bases would help curb the obesity crisis.
RELATED

Accessible and affordable healthy food options are critical for service members to get into or remain in shape, but analysts say the military’s obesity struggles result from more factors than a simple lack of willpower among troops.
Regardless of contributing factors, the small number of troops who have been prescribed drugs like Ozempic must follow a course of treatment that depends on the specific drug prescribed as well as physician instructions, said Peter Graves, a spokesperson for the DHA.
Tricare protocols require patients to use the anti-obesity medication phentermine before others — also approved by the FDA — can be prescribed.
“It’s not as simple [as having] a provider sit in a clinic, recognize the patient would benefit from this medication, order it and hand it to them that same day,” said Army Capt. Taylor Neuman, who co-authored the August study.
There is also the issue of supply and demand. While some companies have announced in recent months that they are lowering the cost of weight-loss drugs, offering them as single-dose vials, the FDA as of August listed limited availability for other anti-obesity medications as a result of increased public demand.
“Shortages have caused a dramatic underutilization rate across all services,” Courtney Manning, a senior research scientist at the American Security Project, told Military Times.
Getting core ingredients for the drugs, some of which are produced abroad, adds complexity to scaling importation and production, she added.
RELATED

Troops using the drugs
The DHA-funded study looked at service member demographics most likely to be prescribed the drug by assessing troops and beneficiaries — 18 to 64 years old — in the military health care system who were prescribed at least one Tricare-approved anti-obesity medication from fiscal 2018 to fiscal 2022.
Those more likely to be prescribed such medications included females, individuals between 30 and 60 years of age, enlisted troops and warrant officers.
Another study published in January in the Medical Surveillance Monthly Report found that sailors, older troops, those working in health care and non-Hispanic Black troops were prescribed the drugs more often than their peers.
The DHA-funded study also found troops and beneficiaries under the age of 20, between 60 and 64 years old and those who identify as “Asian/Pacific Islander or other race” to be associated with lower odds of getting the medications.
Neuman, one of the study’s authors, said more research is needed about what overweight and obese troops are costing the Pentagon.
Additional research is also needed to understand the long-term impact of weight-loss drugs. While short- and medium-term impacts have been looked at, studies to determine whether there are long-term side effects will be necessary, according to Manning.
Despite any potential detriments, demand in the civilian world for weight-loss drugs has surged, even in light of the cost to procure the medications — some starter doses are going for over $1,000 a month, according to a congressional panel.
Such drugs came to prominence back in 2017, when the FDA approved Ozempic, a brand name for the drug semaglutide, which works as a diabetes treatment and has been used to help reduce body weight. Other options followed suit, including Wegovy, also a semaglutide injection, which was approved in 2021.
In 2022, the FDA approved Mounjaro, an injection of the drug tirzepatide, and in 2023, it approved the similar drug Zepbound.
A poll in May by the nonprofit KFF Health found that about one in eight adults said they have taken a GLP-1 agonist, an increasingly popular class of prescription drugs used in part for weight loss in products like Ozempic. Of those polled, 6% said they are currently taking such a drug.
A strong desire among Americans to use the medications aligns with the high prevalence of overweight and obese populations across the country. In 2022, all U.S. states and territories reported an obesity prevalence of more than one in five adults, with the Midwest and South showing the highest prevalence of obesity, according to the Centers for Disease Control and Prevention.
Obesity struggles impact children and young adults as well. About one in six children and adolescents, ages 2 to 19, are overweight, according to data from the National Institute of Diabetes and Digestive and Kidney Diseases, and almost one in five children and adolescents in that same age group are categorized as obese.
And while weight management issues are currently plaguing those in uniform, such problems are also thinning the list of prospective recruits amid an historic recruiting crisis.
Being overweight was recently listed as the number one disqualifying factor among young military applicants, constituting 11% of all disqualifications, according to a 2020 Pentagon study.
“The whole issue of not as many people [qualifying for military service] because of obesity, because of behavioral issues — that’s going to continue,” Army Secretary Christine Wormuth said at the annual Defense News Conference in September.
No uniform policy
To date, the services have not aligned their policies for the use of weight-loss drugs.
The policies that do exist, meanwhile, are “unclear, outdated or restrictive,” the authors of the DHA-funded study wrote.
“These are doctor-prescribed medications and would not be issued directly to troops,” Graves told Military Times. “Service members see a Tricare-
authorized provider who prescribes the medication based on medical necessity.”
Manning said it remains unclear whether troops are asking their providers first about taking such drugs, or whether the providers are suggesting them to the troops.
She noted that she has heard of providers who have prescribed medications to eligible troops for a non-weight-related condition to avoid putting them into a category that would negatively impact their military careers.
Such medications are not routinely prescribed to sailors who enter the Navy’s Body Composition Program — a remedial program for troops who fall short of physical standards — according to Cmdr. Jessica McNulty, spokesperson for the Navy Bureau of Medicine and Surgery, or BUMED.
McNulty added that BUMED is working alongside the Marine Corps on an anti-obesity medication policy that will enable operational medical officers to prescribe them.
“We seek to improve the health and readiness of our fighting force in the safest manner possible and will continue to monitor advancements in research,” she told Military Times.
A review of Coast Guard prescription data from 2018 through the end of 2023 showed similar increases in use of weight-loss medications compared to the other military branches, according to the service. Women, older age groups and senior enlisted and officer groups in the Coast Guard reported a higher number of prescriptions issued.
But Coast Guard officials added that the number of prescriptions distributed may not equate to the number of individuals treated, considering there may be multiple prescriptions for the same individual.
An Air Force official said the service does not prescribe such medications “solely for failing to meet the service’s body composition standards.”
In accordance with Air Force instruction, weight-control medication is not approved for routine use by overweight active duty members, a spokesperson said. The service does, however, allow for the prescription of weight-control medication in select circumstances.
In May 2023, the DHA issued a policy memo that allowed military health care facility providers to prescribe weight-loss medication, an Army spokesperson said.
All Army beneficiaries must meet clinical criteria indicated in the DHA policy and receive prior authorization before receiving anti-obesity or weight-loss medications, the Army spokesperson added. In fiscal 2024, there were 9,464 active duty soldiers who received at least one anti-obesity medication.
Still, more changes around anti-obesity drugs in the military could be on the horizon.
The House-version of the annual defense policy bill, which passed out of the chamber this summer, includes a provision that would require the defense secretary to develop a strategy to align the Pentagon’s obesity-related programs with the classification of obesity as a medically accepted disease.
But the legislation still has a number of hurdles to clear before it becomes law.
Jonathan is a staff writer and editor of the Early Bird Brief newsletter for Military Times. Follow him on Twitter @lehrfeld_media
Read the full article here






![Enclosed MRDS Buyer’s Guide [2024] Enclosed MRDS Buyer’s Guide [2024]](https://i3.wp.com/www.recoilweb.com/wp-content/uploads/2021/08/Sealed-MRDS-3.jpg?w=390&resize=390,220&ssl=1)